I still remember that appointment.
It was January 2025, a follow-up at the polyclinic — something I had been doing every six months since 2023. Each visit felt routine, but each blood test told a slightly different story. My fasting glucose had been creeping up, quietly and persistently.
That day, the doctor looked at my results and said gently:
“Your fasting readings are consistently around 7. You have diabetes.”
My blood test was taken during fasting.
I wasn’t shocked.
Just… still.
Both my parents were diabetic.
I had gestational diabetes in both my pregnancies.
Deep down, I knew this was coming.
But knowing doesn’t make it easier to hear.
What Scared Me Wasn’t Diabetes — It Was What Came After
The doctor explained that I needed to start medication — Metformin.
I nodded and agreed.
But in my mind, a different conversation was happening.
I had heard so many stories:
- The dose keeps increasing
- You start with one pill, then two
- Eventually, it becomes “normal” to depend on medication
That was when I realised something very clearly:
If I don’t do something now, this will only move in one direction.
This wasn’t about refusing medication.
It was about refusing to be passive.

I Wanted to Understand My Body — Not Just Obey Instructions
If I wanted to manage my diabetes properly, I had to monitor my glucose.
But I knew myself.
Finger-pricking.
Writing numbers down.
Doing it multiple times a day.
I wouldn’t last.
So I chose a Continuous Glucose Monitor (CGM) instead.
I signed up for a 14-day trial, not expecting it to change much.
I was wrong.
For the first time, I could see what was happening inside my body:
- Foods I thought were “safe” caused spikes
- Timing mattered as much as portion
- Poor sleep and stress showed up clearly on the graph
Food stopped being something I feared or guessed about.
It became something I could learn from.
Those 14 days gave me insights I had never had in years.
The Support That Changed Everything
After the CGM trial ended, I came across a Glucose Management Programme.
This was the turning point.
I was supported by:
- A GP
- A Dietician
Every day, I logged my meals.
Every day, they reviewed them.
Not to criticise — but to guide.
They helped me understand:
- Why certain foods spiked me
- How to change food combinations and timing
- What to do after a spike instead of panicking
I learned practical, realistic strategies:
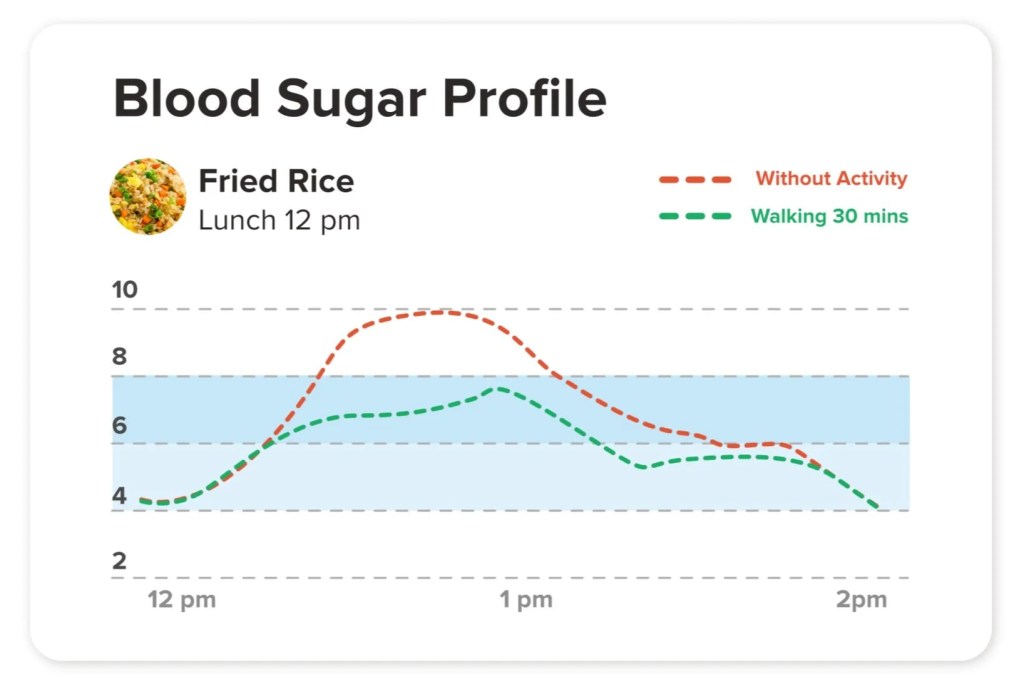
- Walking after meals
- Eating earlier in the evening
- Adjusting portions without feeling deprived
For the first time, diabetes felt manageable — not scary.
When Things Went Too Well
As the weeks went by, my glucose became more and more stable.
Then something unexpected happened.
My readings started going too low — sometimes below 3.
The GP in the programme reviewed my data and said:
“You should stop Metformin.”
Not reduce.
Stop.
I was surprised — and cautious.
The Confirmation That Made It Real
About three months later, I went back to the polyclinic for my scheduled review.
I brought my records.
I shared what I had changed.
The doctor looked through everything and said the same thing:
“You can stop Metformin.”
Hearing it a second time — independently confirmed — made it real.
This wasn’t a fluke.
This wasn’t luck.
My body had responded.
Where I Am Today
Since then, I continue to pay attention to:
- What I eat
- When I eat
- How I eat
Not out of fear —
but out of understanding.
Today, I am in diabetes remission.
Not because I’m extreme.
Not because I’m special.
But because I finally learned how my body works — and respected it.
What I Hope You Take Away From My Story
1. Diabetes is not a personal failure
Genetics, pregnancies, stress, and modern lifestyles all matter.
2. Medication is not the enemy — ignorance is
Metformin helped me stabilise while I learned. Knowledge helped me move forward.
3. Understanding your body changes everything
When you see patterns, change becomes possible.
4. Small, consistent actions work
No crash diets. No punishment. Just daily awareness.
5. Remission is real — and possible
Not the same for everyone, but far more achievable than we are led to believe.
What My Journey Taught Me — And What I Hope You Take Away
When I was first told I had diabetes, I thought the path ahead was fixed — medication, higher doses, and learning to live with “inevitable decline.”
That isn’t how my story turned out.
Through monitoring, guidance, and small but consistent changes, I learned how my body responds — and how much influence I still had over my health. That understanding allowed me to move into remission. But more importantly, it gave me confidence instead of fear.
If you are newly diagnosed, my hope is that you see this as a starting point, not an ending.
If you have been on medication for years, I hope you know this:
You have not failed, and it is not too late. Reversal does not always mean stopping medication. Sometimes it means better stability, fewer spikes, or simply feeling stronger and more in control — and those outcomes matter deeply.
What my journey taught me is this:
- Understanding your body is more powerful than willpower
- Small changes, done consistently, really do add up
- Medication can be a support, not a life sentence
Every body is different. Every journey is personal.
But improvement is almost always possible — at any stage.
Wherever you are today, this is not the end of your story.
It may simply be the moment you start listening to your body — and choosing to care for it, one small step at a time.







Leave a comment